
Benign prostatic hyperplasia (BPH), also called benign enlargement of the prostate (BEP or BPE), is a noncancerous increase in size of the prostate. BPH involves hyperplasia of prostatic stromal and epithelial cells, resulting in the formation of large, fairly discrete nodules in the transition zone of the prostate. BPH involves hyperplasia (an increase in the number of cells) rather than hypertrophy (a growth in the size of individual cells), but the two terms are often used interchangeably, even among urologists.
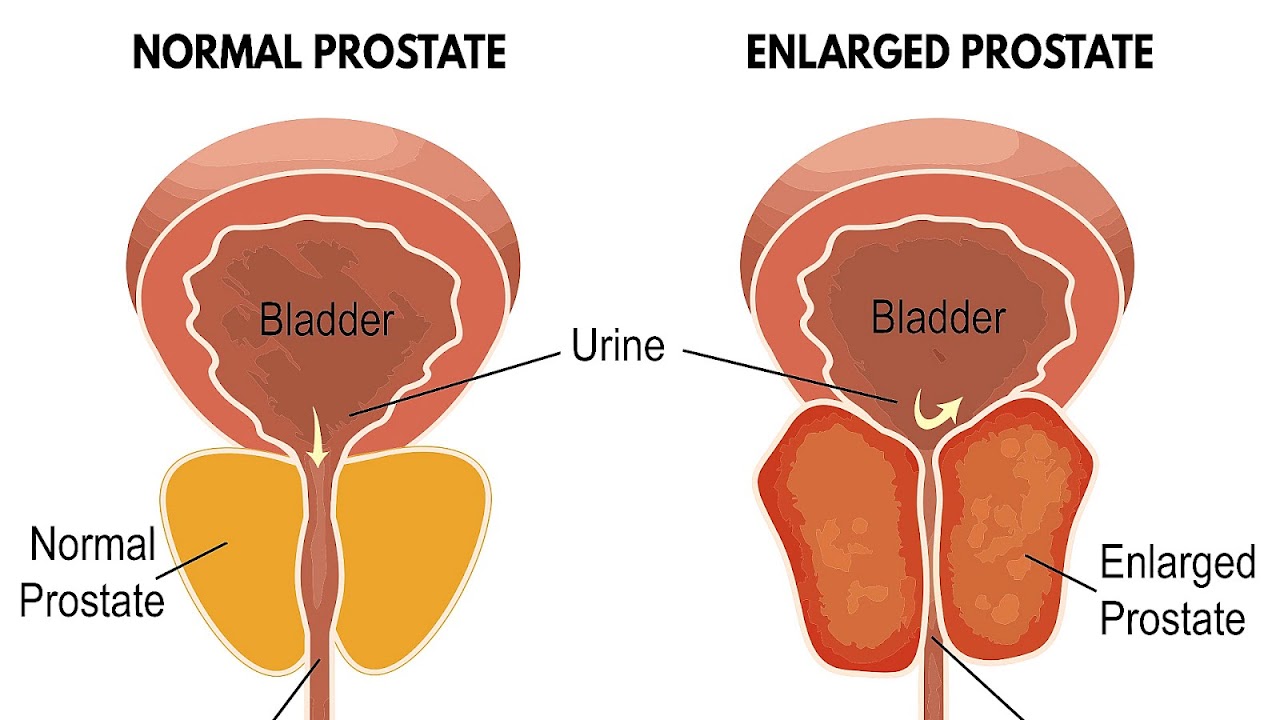
When sufficiently large, the nodules push on and narrow the urethra resulting in an increased resistance to flow of urine from the bladder. This is commonly referred to as "obstruction", although the urethral lumen is no less patent, only compressed. Resistance to urine flow requires the bladder to work harder during voiding, possibly leading to progressive hypertrophy, instability, or weakness (atony) of the bladder muscle. If BPH causes obstruction of the bladder and remains untreated, complications such as recurrent urinary tract infections, bladder stones, and chronic kidney disease (potentially leading to kidney failure) may ensue.
Several treatment options exist to treat BPH, including lifestyle changes, medications, self-catheterization, and surgery. Urinating while in the sitting position may be helpful. Medications commonly used to relieve obstructive symptoms of BPH include ?1-receptor blockers and 5?-reductase inhibitors to reduce pressure on the urethra and allow for easier passage of urine. If conservative treatment with lifestyle modifications and medications fails to relieve the obstructive symptoms of BPH, surgical removal of part of the prostate to relieve compression of the urethra is often necessary. Alternative medicine approaches, such as supplementation with saw palmetto, do not appear to be significantly more effective than placebo.
Adenomatous prostatic growth is believed to begin at approximately age 30. An estimated 50% of men have histologic evidence of BPH by age 50 and 75% by age 80; in 40-50% of these men, BPH becomes clinically significant. BPH was one of the ten most common and costly diseases in men older than 50 years of age in a study in the United States. Although prostate specific antigen levels may be elevated in men affected by BPH because of increased organ volume and inflammation due to urinary tract infections, BPH does not lead to cancer or increase the risk of cancer.
Maps, Directions, and Place Reviews
Signs and symptoms
BPH is the most common cause of lower urinary tract symptoms (LUTS), which are divided into storage, voiding, and symptoms which occur after urination. Storage symptoms include the need to urinate frequently, waking at night to urinate, urgency (compelling need to void that cannot be deferred), involuntary urination, including involuntary urination at night, or urge incontinence (urine leak following a strong sudden need to urinate). Voiding symptoms include urinary hesitancy (a delay between trying to urinate and the flow actually beginning), intermittency (not continuous), involuntary interruption of voiding, weak urinary stream, straining to void, a sensation of incomplete emptying, and terminal dribbling (uncontrollable leaking after the end of urination, also called post-micturition dribbling). These symptoms may be accompanied by bladder pain or pain while urinating, called dysuria.
Bladder outlet obstruction (BOO) can be caused by BPH. Symptoms are abdominal pain, a continuous feeling of a full bladder, frequent urination, acute urinary retention (inability to urinate), pain during urination (dysuria), problems starting urination (urinary hesitancy), slow urine flow, starting and stopping (urinary intermittency), and nocturia.
BPH can be a progressive disease, especially if left untreated. Incomplete voiding results in residual urine or urinary stasis, which can lead to an increased risk of urinary tract infection.
Symptoms can vary throughout the day with mild symptoms after standing or walking and more pronounced symptoms after lying down.

Causes
Hormones
Most experts consider androgens (testosterone and related hormones) to play a permissive role in the development of BPH. This means that androgens must be present for BPH to occur, but do not necessarily directly cause the condition. This is supported by evidence suggesting that castrated boys do not develop BPH when they age. In an unusual study of 26 eunuchs from the palace of the Qing dynasty still living in Beijing in 1960, the prostate could not be felt in 81% of the studied eunuchs. The average time since castration was 54 years (range, 41-65 years). On the other hand, some studies suggest that administering exogenous testosterone is not associated with a significant increase in the risk of BPH symptoms, so the role of testosterone in prostate cancer and BPH is still unclear. Further randomized controlled trials with more participants are needed to quantify any risk of giving exogenous testosterone.
Dihydrotestosterone (DHT), a metabolite of testosterone, is a critical mediator of prostatic growth. DHT is synthesized in the prostate from circulating testosterone by the action of the enzyme 5?-reductase, type 2. DHT can act in an autocrine fashion on the stromal cells or in paracrine fashion by diffusing into nearby epithelial cells. In both of these cell types, DHT binds to nuclear androgen receptors and signals the transcription of growth factors that are mitogenic to the epithelial and stromal cells. DHT is ten times more potent than testosterone because it dissociates from the androgen receptor more slowly. The importance of DHT in causing nodular hyperplasia is supported by clinical observations in which an inhibitor of 5?-reductase such as finasteride is given to men with this condition. Therapy with a 5?-reductase inhibitor markedly reduces the DHT content of the prostate and, in turn, reduces prostate volume and BPH symptoms.
Testosterone promotes prostate cell proliferation, but relatively low levels of serum testosterone are found in patients with BPH. One small study has shown that medical castration lowers the serum and prostate hormone levels unevenly, having less effect on testosterone and dihydrotestosterone levels in the prostate.
While there is some evidence that estrogen may play a role in the cause of BPH, this effect appears to be mediated mainly through local conversion of androgens to estrogen in the prostate tissue rather than a direct effect of estrogen itself. In canine in vivo studies castration, which significantly reduced androgen levels but left estrogen levels unchanged, caused significant atrophy of the prostate. Studies looking for a correlation between prostatic hyperplasia and serum estrogen levels in humans have generally shown none.
In 2008, Gat et al. published evidence that BPH is caused by failure in the spermatic venous drainage system resulting in increased hydrostatic pressure and local testosterone levels elevated more than 100 fold above serum levels. If confirmed, this mechanism explains why serum androgen levels do not seem to correlate with BPH and why giving exogenous testosterone would not make much difference.
Diet
Studies indicate that dietary patterns may affect development of BPH, but further research is needed to clarify any important relationship. Studies from China suggest that greater protein intake may be a factor in development of BPH. Men older than 60 in rural areas had very low rates of clinical BPH, while men living in cities and consuming more animal protein had a higher incidence. On the other hand, a study in Japanese-American men in Hawaii found a strong negative association with alcohol intake, but a weak positive association with beef intake. In a large prospective cohort study in the US (the Health Professionals Follow-up Study), investigators reported modest associations between BPH (men with strong symptoms of BPH or surgically confirmed BPH) and total energy and protein, but not fat intake. There is also epidemiological evidence linking BPH with metabolic syndrome (concurrent obesity, impaired glucose metabolism and diabetes, high triglyceride levels, high levels of low-density cholesterol, and hypertension).
Degeneration
Benign prostatic hyperplasia is an age-related disease. Misrepair-accumulation aging theory suggests that development of benign prostatic hyperplasia is a consequence of fibrosis and weakening of the muscular tissue in the prostate. The muscular tissue is important in the functionality of the prostate, and provides the force for excreting the fluid produced by prostatic glands. However, repeated contractions and dilations of myofibers will unavoidably cause injuries and broken myofibers. Myofibers have a low potential for regeneration; therefore, collagen fibers need to be used to replace the broken myofibers. Such misrepairs make the muscular tissue weak in functioning, and the fluid secreted by glands cannot be excreted completely. Then, the accumulation of fluid in glands increases the resistance of muscular tissue during the movements of contractions and dilations, and more and more myofibers will be broken and replaced by collagen fibers. Progressive fibrosis of muscular tissue and accumulation of fluid are important causes for the expanding of the prostate in benign prostatic hyperplasia.

Pathophysiology
As men age, the enzymes aromatase and 5-alpha reductase increase in activity. Aromatase and 5-alpha reductase are responsible for converting androgen hormones into estrogen and dihydrotestosterone, respectively. This metabolism of androgen hormones leads to a decrease in testosterone but raised levels of DHT and estrogen. Estrogen has a key role in the growth of cells in the prostate and DHT is an anabolic hormone many times more potent than testosterone that when combined, cause a synergy to induce BPH.
Both the glandular epithelial cells and the stromal cells (including muscular fibers) undergo hyperplasia in BPH. Most sources agree that of the two tissues, stromal hyperplasia predominates, but the exact ratio of the two is unclear.:694
Anatomically the median and lateral lobes are usually enlarged, due to their highly glandular composition. The anterior lobe has little in the way of glandular tissue and is seldom enlarged. (Carcinoma of the prostate typically occurs in the posterior lobe - hence the ability to discern an irregular outline per rectal examination). The earliest microscopic signs of BPH usually begin between the age of 30 and 50 years old in the PUG, which is posterior to the proximal urethra.:694 In BPH, the majority of growth occurs in the TZ.:694 In addition to these two classic areas, the peripheral zone (PZ) of the prostate is also involved to a lesser extent.:695 Prostatic cancer typically occurs in the PZ. However, BPH nodules, usually from the TZ are often biopsied anyway to rule out cancer in the TZ.:695 However, prostate cancer most frequently occurs in the PZ rather than the TZ; thus, chippings taken from the PZ are of limited use.

Diagnosis
The clinical diagnosis of BPH is based on a history of LUTS, a digital rectal exam, and exclusion of other causes of similar signs and symptoms. The degree of LUTS does not necessarily correspond to the size of the prostate. An enlarged prostate gland on rectal examination that is symmetric and smooth supports a diagnosis of BPH. However, if the prostate gland feels asymmetrical, firm, or nodular, this raises concern for prostate cancer.
Urinalysis is typically performed when LUTS are present and BPH is suspected to evaluate for signs of a urinary tract infection, glucose in the urine (suggestive of diabetes), or protein in the urine (suggestive of kidney disease). Bloodwork including kidney function tests and prostate specific antigen (PSA) are often ordered to evaluate for kidney damage and prostate cancer, respectively. However, checking blood PSA levels for prostate cancer screening is controversial and not necessarily indicated in every evaluation for BPH. Benign prostatic hyperplasia and prostate cancer are both capable of increasing blood PSA levels and PSA elevation is unable to differentiate these two conditions well. If PSA levels are checked and are high, then further investigation is warranted. Measures including PSA density, free PSA, rectal examination, and transrectal ultrasonography may be helpful in determining whether a PSA increase is due to BPH or prostate cancer. Ultrasound examination of the testes, prostate, and kidneys is often performed, again to rule out cancer and hydronephrosis.
Validated questionnaires such as the American Urological Association Symptom Index (AUA-SI), the International Prostate Symptom Score (I-PSS), and more recently the UWIN score (urgency, weak stream, incomplete emptying, and nocturia) are useful aids to making the diagnosis of BPH and quantifying the severity of symptoms.
Differential diagnosis
Medical conditions
The differential diagnosis for LUTS is broad and includes various medical conditions, neurologic disorders, and other diseases of the bladder, urethra, and prostate such as bladder cancer, urinary tract infection, urethral stricture, urethral calculi (stones), chronic prostatitis, and prostate cancer. Neurogenic bladder can cause urinary retention and cause symptoms similar to those of BPH. This may occur as a result of uncoordinated contraction of the bladder muscle or impairment in the timing of bladder muscle contraction and urethral sphincter relaxation. Notable causes of neurogenic bladder include disorders of the central nervous system such as Parkinson's disease, multiple sclerosis, and spinal cord injuries as well as disorders of the peripheral nervous system such as diabetes mellitus, vitamin B12 deficiency, and alcohol-induced nerve damage. Individuals affected by heart failure often experience nighttime awakenings to urinate due to redistribution of fluid accumulated in swollen legs.
Medications
Certain medications can increase urination difficulties by increasing bladder outlet resistance by increasing smooth muscle tone at the prostate or bladder neck and contribute to LUTS. Alpha-adrenergic agonist medications, such as decongestants with pseudoephedrine can increase bladder outlet resistance. In contrast, calcium channel blockers and anticholinergic medications can worsen urinary retention by promoting bladder muscle relaxation. Diuretic medications such as loop diuretics (e.g., furosemide) or thiazides (e.g., chlorthalidone) can cause or worsen urinary frequency and nighttime awakenings to urinate.
Source of the article : Wikipedia

EmoticonEmoticon